By Loshni S Segaran and Lim Ghee Seong
Introduction
The advent of three-dimensional (3D) printing technology has revolutionized various fields, including dentistry. In particular, the fabrication of removable complete dentures using 3D printing has shown significant promise in improving patient outcomes, reducing production time, and for cost effectiveness. Conventional denture fabrication methods often involve multiple steps and can be time-consuming and labour-intensive. In contrast, 3D printing offers a streamlined approach that can enhance precision and customization.
Advancements in 3D printing materials and techniques have enabled the production of durable and biocompatible dentures that meet patients’ functional and aesthetic needs. Study has demonstrated that 3D-printed dentures can achieve comparable or superior fit and comfort to conventional dentures (Anadioti et al., 2020). Additionally, the digital workflow associated with 3D printing allows for the easy replication and modification of denture designs, facilitating better patient management and follow-up care.
The present case report explores the clinical application and outcomes of using 3D printing technology to fabricate a removable complete denture for a patient with dementia. The report highlights the procedural steps, materials used, and the resulting benefits observed in terms of fit, comfort, and patient satisfaction. Although the number of appointments followed the usual workflow, the use of 3D printing provided significant advantages in terms of accuracy and customization of the dentures.
For dementia patients, 3D printing of dentures offers specific advantages. Dementia patients often experience difficulties with traditional denture procedures due to their cognitive impairments. The digital workflow can help maintain consistent denture quality and fit, which is crucial for the comfort and oral health of dementia patients (Arai et al., 2021). Furthermore, replicating and modifying existing dentures digitally ensures that replacements can be made quickly if dentures are lost or damaged, which is particularly beneficial for patients with dementia who may misplace their dentures frequently. By presenting this case, we aim to contribute to the growing body of evidence supporting the efficacy of 3D-printed dentures and encourage further adoption of this innovative approach in dental practice.
Case Description
An 82-year-old Chinese woman was referred to the Prosthodontic Postgraduate Clinic due to persistent pain in her lower jaw caused by her existing denture. Upon examination, it was found that she was edentulous in both the upper and lower arches, wearing ill-fitting cobalt-chrome complete dentures. The definitive treatment plan was to provide her with new complete dentures to alleviate her discomfort and restore oral function.
Patient, a retired food stall owner, has been without natural teeth for 30 years. Her current dentures, which were fabricated in a private clinic, have been in use since then. Over the past three months, she has experienced on-and-off pain in her gums, significantly affecting her ability to chew and swallow food. This situation has caused considerable discomfort and frustration for her.
Her medical history is extensive, including hypertension managed with Perindopril, hypercholesterolemia controlled by Atorvastatin, diabetes mellitus treated with Metformin, and moderate dementia diagnosed two years ago. Additionally, she had her thyroid removed 20 years ago and takes Thyroxine. Despite these medical conditions, she maintains a non-smoking lifestyle, does not consume alcohol, and has no specific dietary preferences. She is married with four children and receives assistance from her daughter and a helper for her daily oral hygiene routine, which includes using a soft-bristle toothbrush and fluoridated toothpaste.
During the clinical examination, several key observations were made. Externally, her face appeared symmetrical, her lips were competent, and she had a normal mouth opening range of 25-35mm. Clicking sounds were noted in both the left and right temporomandibular joints, but there were no palpable or tender submandibular lymph nodes, and her skeletal profile was classified as Class I.
Intraoral examination revealed a 1x1mm multiple ulcer on the right labial mucosa and lingual region. The maxillary residual ridge (Figure 2) showed mild resorption (Order 5), a regular contour, and flabby mucosa in the anterior region, while the mandibular residual ridge (Figure 3) displayed extreme resorption (Class 6) with firm mucosa (Atwood 1971).



The examination of her existing dentures (Figure 4 and 5) highlighted several issues. The maxillary denture had poor aesthetics but good retention and stability, although it exhibited discrepancies in occlusion. The mandibular denture, on the other hand, had poor aesthetics, retention, stability, and extension. Both dentures had fair hygiene, and the patient reported using denture adhesive, and she claimed the adhesive was ineffective.


Given these findings, the diagnosis included edentulous maxilla and mandible and denture-related traumatic ulcers. The primary treatment goals were to restore oral function and improve soft tissue health. The treatment plan was structured into three phases: preparatory, restorative, and maintenance.
In the preparatory phase, oral hygiene maintenance was emphasized. She was advised to discontinue using her old dentures to allow her tissues to heal, and oral aids were provided to promote the healing of the ulcers. The restorative phase involved fabricating new complete dentures for both the maxilla and mandible using 3D Printing technology. This option was chosen for the advantages of digital precision.
The treatment process combined conventional and digital techniques. Primary impressions were made using standard non-perforated metal stock trays, with impression compound material for the maxillary arch and silicone putty for the mandibular arch. The stone cast was poured, and a secondary impression was taken using polyvinyl silicone material. A perforated special tray was used for the secondary impression to stabilize the maxillary anterior flabby ridge and minimize distortions. These impressions were digitized with a laboratory scanner to create a digital cast, ensuring correct vestibular sulcus dimensions for better retention through peripheral sealing. A perforated tray was used for the secondary impression to stabilize the flabby ridge and minimize distortions.

Record blocks were fabricated using light cure custom tray base plate and wax rims. Then, jaw relation registration was performed. The upper and lower master stone casts and bite registration were extra orally digitalized with a laboratory scanner (Figure 7).

The dentures were designed, and artificial teeth setting up were arranged using CAD software. A lingualised occlusion scheme was utilized for this patient. The designed data was obtained and transported to 3D printer to fabricate the try in denture using digital light projection (DLP).


During try-in stage, the denture base extensions, retention, stability, occlusion and phonetics was assessed. Later the data was sent again to the 3D printer to fabricate the 3D resin denture base (NextDent Base, Netherlands), resin teeth set was fabricated based on the scan data of the bite registration and bonded to the denture base. All laboratory works performed at Apex Digital Laboratory.
On the day of denture delivery, post-insertion evaluations confirmed satisfactory retention, stability, extension, and occlusion, achieving lingualised bilateral balanced occlusion. Denture occlusion was checked by chewing articulating paper on both sides and no heavy localised occlusal contacts were found. The patient didn’t complain of occlusal interference and lesserocclusal adjustments were necessary. The retention and stability of the digital complete denture were assessed using Kapur’s method (1967). For evaluating denture retention, the thumb and index fingers were placed on the labial and lingual sides of the central incisor teeth. A vertical pulling force was applied along the path of insertion. Stability was assessed by positioning the thumb and index fingers on the buccal surfaces of the premolar teeth, and the denture was moved horizontally, anteroposteriorly, and mediolaterally. The retention and stability were recorded as very good.
<< Back to Contents Menu
EDITOR’S PAGE | ADVISORY BOARD | NEWS | PRODUCTS | COVER FEATURE | CLINICAL | PROFILE | EXHIBITIONS & CONFERENCES | PRACTICE MANAGEMENT

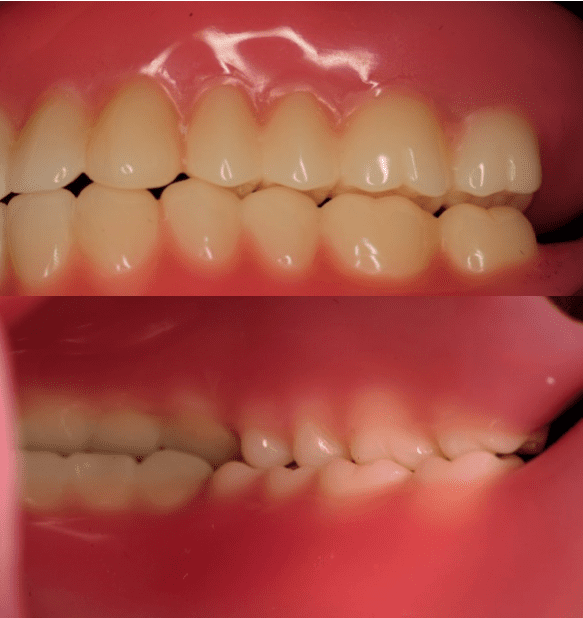

Fig 12: Intraoral views of upper and lower 3D printing complete denture in position

Discussion
Digital denture processing provides several benefits, including speed, efficiency, and the ability to store captured information. It allows for the seamless transfer of digital images between the dental office and the laboratory (Kim, 2013). The CAD system facilitates virtual planning and designing of prostheses with consistency, and the design data can be saved for future refabrication or modification if necessary. Additionally, the total time required for prosthesis fabrication is significantly reduced by eliminating certain laboratory processes, highlighting the superiority of the digital method over traditional approaches (William, 2004).
The case of an 82-year-old woman with dementia underscores the significant advantages and some challenges of using 3D printing technology for complete denture fabrication. Traditional denture methods are often cumbersome and time-consuming, particularly for patients with cognitive impairments who may find multiple dental visits and lengthy procedures difficult to manage. In this instance, 3D printing offered notable benefits in terms of precision, customization, and overall patient comfort.
One of the most notable advantages of 3D printing technology is its ability to produce highly precise and customized dentures. The digital workflow allowed for accurate replication of the patient’s oral structures, ensuring a better fit and enhanced comfort. This precision is particularly crucial for patients with extensive ridge resorption, as seen in this case. Additionally, the digital workflow minimized the number of dental appointments, a significant advantage for dementia patients who may experience anxiety or confusion with repeated visits. Digital impressions and cast creation reduced the need for multiple physical fittings, streamlining the process.
The fit and comfort of the 3D-printed dentures were superior to the patient’s previous cobalt-chrome dentures. The use of NextDent Base resin material provided a biocompatible and durable solution. Post-insertion evaluations showed satisfactory retention and stability, with minimal occlusal adjustments required. The patient reported no discomfort, highlighting the effectiveness of 3D printing in achieving a functional and comfortable prosthesis. Moreover, the digital nature of the workflow allows for easy storage and retrieval of denture designs, which is particularly beneficial for dementia patients who may frequently misplace their dentures, ensuring that replacements can be made efficiently.
Despite these benefits, some challenges warrant consideration. Although advancements in 3D printing materials have been significant, their long-term durability and wear resistance compared to traditional materials need further study. Ensuring that the materials used are biocompatible and capable of withstanding the forces of mastication over time is essential for the success of 3D-printed dentures. Additionally, the initial cost of setting up a 3D printing system and the need for specialized training can be barriers for some dental practices. However, the long-term benefits and potential cost savings in terms of reduced chair time and enhanced patient satisfaction may outweigh these initial investments.
Denture care for individuals with dementia presents significant challenges due to cognitive impairments that affect their ability to maintain oral hygiene, leading to a higher risk of oral health issues like infections and discomfort. The introduction of 3D-printed dentures offers a compelling solution by providing highly customized and precise fittings, particularly beneficial for dementia patients who may experience discomfort with traditional dentures. These customized dentures can reduce the occurrence of oral sores and enhance overall comfort, which is critical for ensuring that patients consistently wear their dentures. Furthermore, the ease of reproducing dentures with 3D printing technology addresses the common issue of lost or damaged dentures in dementia care. By combining 3D-printed dentures with effective caregiver education on proper denture maintenance, the overall oral health and quality of life for dementia patients can be significantly improved (Fujisawa et al., 2007).
Conclusion
This case report demonstrates the significant potential of 3D printing technology in the fabrication of complete dentures, especially for patients with complex medical histories and cognitive impairments like dementia. The precision, customization, and efficiency of 3D printing offer considerable advantages over traditional methods, leading to improved patient outcomes and satisfaction. While challenges such as material limitations and initial costs exist, the benefits of reduced appointment times, enhanced fit and comfort, and easy replication make 3D printing a promising approach in modern prosthodontics.
Further research and advancements in 3D printing materials and techniques will continue to enhance the viability and effectiveness of this technology, potentially making it the standard of care in the future. For dental practitioners, embracing digital workflows and 3D printing technology can significantly improve patient management and outcomes, particularly for those with special needs such as dementia.
References
- Arai, K., Tanaka, Y., Matsuda, S., Okamura, T., Iwayama, K., & Ono, Y. (2021). Complete Denture Fabrication Using Digitally Fabricated Copy Dentures for a Patient with Moderate Dementia. Case Reports in Dentistry, 2021.
- Atwood, D. A. (1971). Reduction of residual ridges: a major oral disease entity. Journal of Prosthetic Dentistry, 26(3), 266-279.
- Kapur, K. K. (1967). A clinical evaluation of denture adhesives. The Journal of prosthetic dentistry, 18(6), 550-558.
- Kim, S. Y., Kim, M. J., Han, J. S., Yeo, I. S., Lim, Y. J., & Kwon, H. B. (2013). Accuracy of dies captured by an intraoral digital impression system using parallel confocal imaging. International Journal of Prosthodontics, 26(2).
- Williams, R. J., Bibb, R., & Eggbeer, D. (2004). CAD/CAM in the fabrication of removable partial denture frameworks: a virtual method of surveying 3D scanned dental casts. Quintessence J Dent Technol, 2, 268-76.
- Fujisawa, T., Yokoyama, A., Muramatsu, M., Kimura, Y., Kurozumi, A., Kobayashi, I., Sano, H., Totsuka, Y., & Fukushima, K. (2007). Fitting complete dentures after multiple tooth extraction in a patient with severe dementia.. Special care in dentistry : official publication of the American Association of Hospital Dentists, the Academy of Dentistry for the Handicapped, and the American Society for Geriatric Dentistry, 27 5, 187-90 . https://doi.org/10.1111/J.1754-4505.2007.TB00344.X.
Acknowledgement:
Special thanks to Apex Digital Laboratory for the great support in printing the 3D printed dentures.

Dr. Loshni S. Sagaran is currently a prosthodontic postgraduate resident in the Department of Restorative Dentistry at Universiti Malaya. She obtained her Bachelor of Dental Surgery (BDS) from VMU, India, in 2013. Following her graduation, she served as a dental officer for 10 years under the Ministry of Health Malaysia, working in various states, including Pahang and W.P Kuala Lumpur. In 2019, she obtained the Membership of the Royal College of Surgeons of Edinburgh (MFDS RCSEd). She was awarded a scholarship from the Ministry of Health to specialize in prosthodontics. Dr. Loshni completed her Master of Oral Science (MOSc) in 2023 at Universiti Malaya and is currently pursuing her clinical Doctorate in Prosthodontics (DrProstho)

Associate Professor Dr. Lim Ghee Seong graduated with a Bachelor of Dental Surgery from University of Malaya, Kuala Lumpur in 2008. He then pursued his Master in Clinical Dentistry, specializing in Restorative Dentistry at Newcastle University, Newcastle Upon Tyne, United Kingdom, where he graduated with distinction. He has also been awarded the International Training Fellowship (Prosthodontics) from the Royal College of Surgeons (England). His passion for teaching then led him to join the Faculty of Dentistry, University of Malaya and he has since become a valuable lecturer and clinical specialist in prosthodontics in the Department of Restorative Dentistry. He is currently the program coordinator for Master of Oral Sciences in Restorative Dentistry, he was the year coordinator for removable prosthodontic undergraduate year 5, head of the undergraduate module on occlusion and one of the multidisciplinary team for the TMD clinic. He has previous membership in the British Society for Restorative Dentistry, assistant secretary for the Malaysian Association of Aesthetic Dentistry, currently a lifetime member and vice president of the Malaysian Association for Prosthodontics. Currently, he is also the examiner for the Restorative Specialty Membership Examinations, Royal College of Surgeons, England. He has authored and co-authored handful of both local and international journal articles. His research interest is in clinical removable prosthodontics, regenerative dentistry, dental material and temporomandibular joint disorder (TMD).
The information and viewpoints presented in the above news piece or article do not necessarily reflect the official stance or policy of Dental Resource Asia or the DRA Journal. While we strive to ensure the accuracy of our content, Dental Resource Asia (DRA) or DRA Journal cannot guarantee the constant correctness, comprehensiveness, or timeliness of all the information contained within this website or journal.
Please be aware that all product details, product specifications, and data on this website or journal may be modified without prior notice in order to enhance reliability, functionality, design, or for other reasons.
The content contributed by our bloggers or authors represents their personal opinions and is not intended to defame or discredit any religion, ethnic group, club, organisation, company, individual, or any entity or individual.