By Pol. Maj. Dr. Ratchaphat Khomprang and Dr. Sunporn Namano
Currently, there is increased demand for achieving cosmetic appeal and natural-looking results in anterior restorations. Many patients have high expectations regarding the appearance of their teeth, making it challenging for dentists to manage and meet these expectations, especially in the aesthetic zone. Various treatment options are available for anterior restorations, with dental veneers being widely used to enhance a patient’s appearance. Among these, ceramic veneers are considered one of the most aesthetic materials [1]. A thorough treatment plan that includes smile design, wax-up, and mock-up is essential for giving patients a clear visualisation of the final appearance from the onset of the treatment process, ensuring progress toward the expected aesthetic outcome.
This article presents the case of a 34-year-old Thai woman who visited a dental clinic with the primary concern of wanting to correct her teeth’s appearance. She desired a more pleasing smile, because she felt her teeth were irregularly shaped and discoloured. The patient requested aesthetic, natural-looking teeth with improved alignment and sought simultaneous treatment for her upper and lower teeth. She had approximately one month available for treatment before returning to Myanmar. Although she had previously undergone in-office tooth bleaching and orthodontic treatment, she declined further orthodontic adjustments to correct the arrangement of her teeth.



Extra- and intra-oral examinations revealed that the patient had a low smile line showing the upper and lower second premolars and an asymmetrical lower lip (Figure 1), the midline of the upper teeth was shifted ~0.5 mm to the left side and that of the lower teeth was shifted ~1 mm to the left, improper tooth proportion, asymmetrical tooth axis between the right and left side, overly prominent central incisors (tooth 11, 21), tooth 12 not symmetrical to tooth 22, occlusal plane canting to the right side, black triangles on the upper and lower teeth, tapered tooth shape, yellowish tooth color with white spot lesions, edge to edge occlusion between tooth 22 and 32 (minor tooth position problem), and normal buccal corridor dimensions (Figure 2). Before starting treatment, a panoramic radiograph was utilized to evaluate the overall bone support level and rule out any abnormal findings (Figure 3).
Dental veneers are indicated for: 1) discolored teeth, 2) fractured and worn teeth, 3) abnormal tooth structure, 4) correcting minor tooth malposition, and 5) restoring fractured crowns and bridge facings [2, 3]. Several clinical investigations revealed that 80–100% of patients are satisfied with their veneer treatment. Multiple studies demonstrated that ceramic veneers have a 12-year survival rate [3]. Based on the patient’s problem list and esthetic expectation, dental ceramic veneers were selected as a suitable method for treating this patient.

The patient’s examination results were used in the smile design process. An RED proportion of 0.76 was used to decrease the prominence of the central incisors. To increase the contact point areas in the upper and lower teeth and eliminate the black triangles, a square tapered tooth shape was preferred instead of the existing tapered shape (Figure 4). The occlusal canting was corrected to be parallel with the inter-pupillary line. Moreover, the incisal edges were made to follow the lower lip curvature for a more natural appearance. Before starting the irreversible stage of tooth preparation, we used a mock-up for better visualisation and discussed the results with the patient to help her fully understand and obtain her approval for the proposed treatment outcome.
After the mock-up step was finished, the tooth preparation was done directly from the mock-up and a silicone jig was used to check the available veneer thickness, which should be 0.5-0.7 mm at the labial surface [3, 4]. The jig helped prevent tooth over-preparation. However, to correct the minor tooth malposition and close the black triangles, the preparation depth needed to be more than 0.7 mm, but still in the enamel layer in those areas. In this case, the incisal edge was reduced to prevent fracture from occlusal stress on the incisal third and to obtain adequate restoration space for incisal translucency and characteristics [3].
The veneer margin location is an essential factor that affects the long-term stability and esthetic outcome. The veneer margin was located on enamel to establish stable long-term bonding [5]. The preparation margin was slightly under the gingival margin to hide the transition zone. Additionally, the proximal elbow preparation is important because it needs to be sufficient to achieve an esthetic outcome in proximal areas.
Determining the tooth shade is an important step, especially to communicate with the dental technicians. The final preferred shade and the stump shade were determined under natural light. To record the details of the patient’s teeth, stump shade, and shade matching, intra-oral photographs were taken in good lighting conditions.
The high-quality digital photographs were an important tool to fill the communication gap between the dentist and dental technicians, which is one of the most important factors contributing to the success of esthetic restorative outcomes [6]. In this case, the final shade chosen was OM3 (Vita3D master shade guide), and the stump shade was ND2 (Natural die shade guide). Next, the final impression was taken using silicone with a double mixed double impression technique, facebow transfer was performed, and the bite registration was taken in centric occlusion. A well-designed temporary restoration is crucial in stabilizing the gingival margin, preventing gingival inflammation, and preventing tooth sensitivity. It also confirms the final tooth form and shape with the patient.




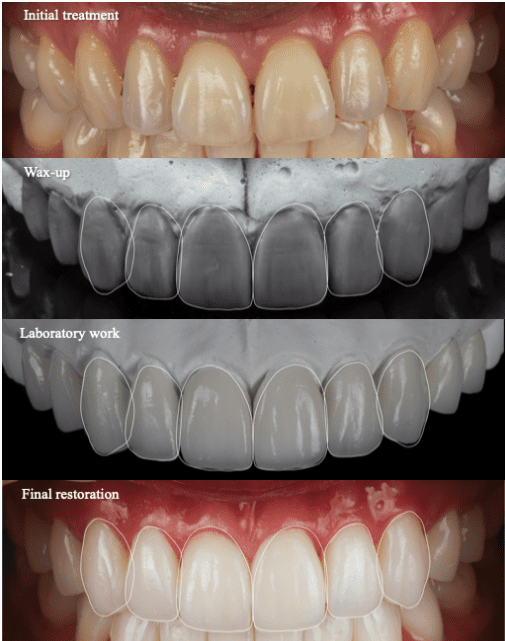
The strongest glass-ceramic material is lithium disilicate glass ceramic, which is ~3-4-fold stronger than other glass-rich ceramics [7]. The heat-press group of ceramic materials produce better marginal and internal adaptation results than computer-aided design and computer-aided milling (CAD-CAM) [8,9]. To provide a natural appearance, the veneer must have incisal characteristics and translucency (Figure 5,6,7). Thus, in this case, lithium disilicate glass ceramic (IPS E.max press (MT)) materials were used.
<< Back to Contents Menu
EDITOR’S PAGE | ADVISORY BOARD | NEWS | PRODUCTS | COVER FEATURE | CLINICAL | PROFILE | EXHIBITIONS & CONFERENCES | PRACTICE MANAGEMENT




The clear shade of light-cured resin cement, which excludes tertiary amine, was utilised for long-term colour stability [10] because the patient expressed satisfaction with the final shade of the veneers after being tried in. As compared with immediately after cementation (Figure 8, 9), and after one-month recall (Figure 10, 11, 12, 13, 14), the colour was stable.
The long laboratory and clinical process led to the conclusion that aesthetic restoration in aesthetic zone presents greater challenges than other situations. Before beginning treatment, dentists must be careful to examine the patient’s list of problems and be able to visualise the potential results and options. Each patient’s subjective preference for cosmetics is individualised. Thus, the key to achieving the ideal aesthetic result for each patient is to identify the root cause of their chief complaints and utilise all available knowledge in every step of the treatment procedure.
References
- Calamia JR. The etched porcelain veneer technique. N Y State Dent J. 1988;54(7):48-50.
- El-Mowafy O, El-Aawar N, El-Mowafy N. Porcelain veneers: An update. Dent Med Probl. 2018;55(2):207-11.
- Alothman Y, Bamasoud MS. The Success of Dental Veneers According To Preparation Design and Material Type. Open Access Maced J Med Sci. 2018;6(12):2402-8.
- Ferrari M, Patroni S, Balleri P. Measurement of enamel thickness in relation to reduction for etched laminate veneers. Int J Periodontics Restorative Dent. 1992;12(5):407-13.
- Zhu J, Gao J, Jia L, Tan X, Xie C, Yu H. Shear bond strength of ceramic laminate veneers to finishing surfaces with different percentages of preserved enamel under a digital guided method. BMC Oral Health. 2022;22(1):3.
- Griffin JD, Jr. Excellence in photography: heightening dentist-ceramist communication. Dent Today. 2009;28(7):124-7.
- Wendler M, Belli R, Petschelt A, Mevec D, Harrer W, Lube T, et al. Chairside CAD/CAM materials. Part 2: Flexural strength testing. Dent Mater. 2017;33(1):99-109.
- Mously HA, Finkelman M, Zandparsa R, Hirayama H. Marginal and internal adaptation of ceramic crown restorations fabricated with CAD/CAM technology and the heat-press technique. J Prosthet Dent. 2014;112(2):249-56.
- Azar B, Eckert S, Kunkela J, Ingr T, Mounajjed R. The marginal fit of lithium disilicate crowns: Press vs. CAD/CAM. Braz Oral Res. 2018;32:e001.
- Ural Ç, Duran İ, Tatar N, Öztürk Ö, Kaya İ, Kavut İ. The effect of amine-free initiator system and the polymerization type on color stability of resin cements. J Oral Sci. 2016;58(2):157-61.

Pol. Maj. Dr. Ratchaphat Khomprang, the founder and director of Dr. Sax Dental Clinic, is an experienced dentist with an enthusiasm for cosmetic dentistry. He has been working full-time at Thailand’s Police General Hospital. In addition, his occupation includes being a dentist and member of the Royal Thai Police. His commitment to helping patients achieve the perfect smile has always motivated him. He has always had a dedication for learning and an interest in implant and cosmetic dentistry.
In 2019, Dr. Rachaphat graduated with a Bachelor of Science degree in Doctor of Dental Surgery (DDS) with first class honors and the gold medal from The Rangsit University in Thailand. He has completed the following programs: Certificate training program in Digital and Esthetic Restoration, Private Dentist Association of Thailand (PDAT), Thailand; Continuing Education programs in Implant Dentistry of the Faculty of Dentistry, Mahidol University, Thailand; Advanced Implantology Surgery and Bone Regeneration, UIC Barcelona, Spain; Postgraduate Diploma in Orthodontics & Dentofacial Orthopaedics (PG Dip.), London Dental Institutes (LDi.), United Kingdom. He currently studies in Chulalongkorn University’s international program for Master of Science in Esthetic Restorative and Implant Dentistry at the Faculty of Dentistry.

Dr. Sunporn Namano is a Prosthodontist with 10 years of working experience. She is a well-qualified dental specialist that focusses in treating patient, doing research and teaching dental students in areas of Prosthodontics, Digital Dentistry, Implant Dentistry, Esthetic Dentistry, and Full Mouth Rehabilitation. She’s committed in providing the best treatment and experience for her patients and students.
After graduating Doctor of Science in Dentistry (DScD) and Certificate of Advanced Graduate Study (CAGS) in Prosthodontics from Boston University Henry H. Goldman School of Dental Medicine, Boston, USA in 2023, she has been serving as a full-time lecturer and instructor in the Master of Science Program in Implant and Esthetic Dentistry (International Program), Faculty of Dentistry, Chulalongkorn University. Her part-time occupation is working as a Prosthodontist in her family’s dental private practice, Sunphat Dental Clinic.
The information and viewpoints presented in the above news piece or article do not necessarily reflect the official stance or policy of Dental Resource Asia or the DRA Journal. While we strive to ensure the accuracy of our content, Dental Resource Asia (DRA) or DRA Journal cannot guarantee the constant correctness, comprehensiveness, or timeliness of all the information contained within this website or journal.
Please be aware that all product details, product specifications, and data on this website or journal may be modified without prior notice in order to enhance reliability, functionality, design, or for other reasons.
The content contributed by our bloggers or authors represents their personal opinions and is not intended to defame or discredit any religion, ethnic group, club, organisation, company, individual, or any entity or individual.