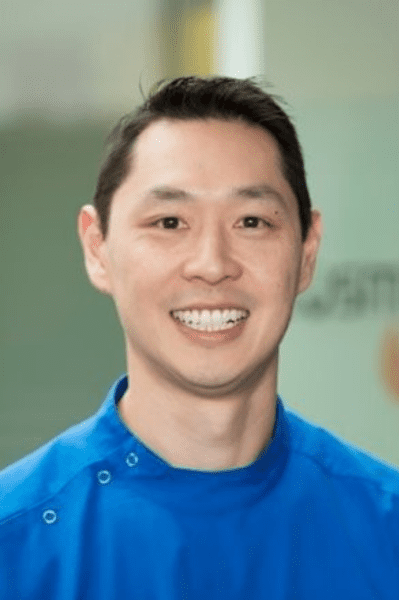
Dr. Jason Pang is an accomplished professional in the field of dentistry, boasting a distinguished academic background. He earned a Bachelor of Science (Biomedical Science) with a University Medal in 1994 from the University of Technology, Sydney, followed by an Honours degree in 1995, during which he conducted research on Cardiac Arrhythmia drugs. In 2002, Dr. Pang furthered his education by completing a Bachelor of Dental Surgery at The University of Sydney. Known as “the Smile Architect”, the expertise of the Neutral Bay dentist in Sydney extends across various dental disciplines, encompassing areas such as teeth whitening, smile makeovers, dental implants, and gum and periodontal treatment. Beyond his dental practice, Jason Pang is the proud proprietor of Mindflux, a center of excellence in dentistry. He is also an accomplished author and a distinguished international speaker. His extensive experience and contributions in the field of dentistry reflect his commitment to advancing the art and science of oral care.
Cancer can be treated in many ways but the therapies may come with side effects. The most common complication of radiotherapy (RT) of head and neck (H&N) cancer is oral mucositis (OM)1. These are the inflammatory and/or ulcerative lesions of the mouth and throat resulting in pain, dysphagia and impairment of speech2. It is also a lesser complication of haemopoietic stem cell transplantation (HSCT) and chemotherapy3.
Mucositis occurs in 20–40% of the patients receiving anti-cancer treatments for solid tumours, 60–80% of patients undergoing HSCT, and is experienced by almost all patients receiving radiotherapy for head and neck (H&N) cancers4.
In Australia, standard care currently for OM is symptomatic, directed towards pain management and the prevention of infection5,6. Pain control usually requires the use of topical anaesthetic and in severe cases may require opioid analgesics7–10. Additionally, the pain and discomfort may require enteral or parenteral nutrition and reduces the patient’s quality of life in terms of their ability to socialise, speak and perform normal daily functions8,9,11,12. Mucositis also has a considerable economic impact due to costs associated with symptoms management, nutritional support, management of secondary infection, and abrupt and/or extended hospitalisation13,14. It is therefore a highly significant and sometimes dose-limiting factor of the toxicity of cancer therapy.
Following successful cancer therapy, the most common long-term complication is xerostomia due to salivary gland hypofunction with a prevalence of 93% during RT and 74%-85% following RT15. Not only does xerostomia significantly impair patients’ quality-of-life (QoL) but it also has important medical sequelae, incurring high medical and dental costs15.
While there are saliva substitutes and sialagogic agents to stimulate saliva, they are unable to replace the antibacterial and immunological components of the saliva so high caries risk and oral infections become more prevalent16.
The biological effects of photobiomodulation (PBM) therapy were discovered by Endre Mester in 196717. PBM therapy aims to treat or prevent oral mucositis complications by reducing inflammation, reducing cellular damage, increasing cell metabolism and promoting healing18. It was first used for the prevention and treatment of radiation-induced mucositis in 1999 by Bensadoun and co-workers19.
According to systematic reviews and meta-analyses, photobiomodulation therapy has been shown to enhance survival rates, decrease the occurrence and intensity of mucositis, shorten its duration, alleviate pain, mitigate xerostomia, minimize interruptions in cancer treatment, and enhance nutritional outcomes20–23. These results were shown in both adult and paediatric populations24,25.
A prospective RCT of PBM for OM showed statistically significant differences between the groups from week 5 of oncological treatment; 73% of the laser group showed normal mucosa (Table 1), while in the control group, 20% showed grade 0 mucositis and 40% showed grade 2 mucositis (P < 0.01)26.
| Grade | Description |
| Mild | |
| 0 (none) | None, normal mucosa |
| I (mild) | Oral soreness, erythema, no ulceration |
| II (moderate) | Oral erythema, ulcers, solid diet tolerated |
| Severe | |
| III (severe) | Oral ulcers, extensive erythema, liquid diet only |
| IV (life-threatening) | Oral feeding not possible, requires parenteral nutrition |
Photobiomodulation therapy is currently the recommended treatment for preventing oral mucositis when using certain treatment modalites, as recently outlined in the clinical practice guidelines of the Multinational Association for Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO)27. Expanding on these recommendations, the World Association of photobiomoduLation Therapy (WALT) group outlines evidence and prescribes PBM treatment parameters for prophylactic and therapeutic use in supportive care of radiodermatitis, dysphagia, xerostomia, dysgeusia, trismus, mucosal and bone necrosis, lymphedema, hand-foot syndrome, alopecia, oral and dermatologic chronic graft-versus- host disease, voice/speech alterations, peripheral neuropathy, and late fibrosis amongst cancer survivors28.
The challenge faced by the patient is that the treatment should ideally be administered every 48 hours, or practically, three times per week. However, maintaining a regular attendance schedule can pose challenges in addition to their hospital visits.
Both lasers and LEDs can be used to perform photobiomodulation but the use of laser often results in shorter treatment times and immediate pain relief. The advantage of LEDs are that they can be self-administered by the patient at home, unlike laser PBM which needs to be performed by a certified laser practitioner.
Case Report 1
A 79-year old male attended our clinic to have PBM therapy in conjunction with radiochemotherapy. A prophylactic protocol for OM commenced on the day of cancer treatment and continued three times a week for the duration of his cancer treatment. 650 nm laser PBM therapy was done around the mouth in accordance with dosimetry parameters recommended29,30. The patient was able to remain mucositis-free for the duration of his cancer treatment (Fig. 1)

Case Report 2
A 64-year old male presented to our clinic with large ulcerated lesions on his cheek, tongue and lip due to chemotherapy for pancreatic cancer. This marked his second round of chemotherapy and the ulcers had worsened compared to the previous round. As his chemotherapy was scheduled every 3rd week, some ulcers were not able to heal completely resulting in fibrotic lesions. 1064 nm Nd:YAG laser PBM therapy was performed 3x weekly to assist with pain and accelerate healing. A combination of intra- and extraoral treatment was performed as mouth opening was restrictive due to trismus (Fig. 2). Symptomatic relief was noticed during the session and faster healing was observed by the patient (Fig. 3). Many ulcers showed complete healing prior to the next round of chemotherapy (Fig. 4). PBM therapy continued until the cessation of chemotherapy.



Case Report 3
A 61-year old male presented to our clinic with a large cheek ulcer despite self-administering home LED photobiomodulation. The patient was undergoing radiotherapy for tonsillar cancer and required daily opioids for pain management. 1064 nm Nd:YAG laser PBM therapy was administered 3x weekly as an adjunct to his home therapy. The patient found immediate relief from the therapy and healed rapidly (Fig. 5). Furthermore, the patient was concurrently dealing with radiation dermatitis on his neck, which had nearly fully healed within 12 days following a 70 Gy radiation treatment administered over a span of 7 weeks. Typically, radiation dermatitis reaches its peak around two weeks after the completion of radiotherapy (Fig. 6).


Case Report 4
A 71-year old male presented to our clinic with painful ulceration of his tongue and cheek. These lesions appeared toward the end of his radiotherapy despite home photobiomodulation with LEDs. Both intraoral and extraoral 1064 nm Nd:YAG laser PBM therapy was performed 3x weekly (Fig. 7) and provided immediate relief. Therapy continued until the lesions resolved.

1064 nm Nd:YAG laser PBM of the cheek (D)
In conclusion, LED and laser photobiomodulation can provide prophylactic and therapeutic relief for the complications of cancer therapy. They can be used as a monotherapy or in combination to modulate pain, accelerate healing and reduce inflammation using complementary wavelengths.
As international guidelines endorse the use of photobiomodulation therapy and lasers become more readily accessible in dental clinics and hospitals, an increasing number of people with cancer can hope to avoid the debilitating complications associated with cancer treatments.
References
1. Basile D, Di Nardo P, Corvaja C, et al. Mucosal injury during anti-cancer treatment: From pathobiology to bedside. Cancers (Basel). 2019;11(6):1-23. doi:10.3390/cancers11060857
2. M. Thomson, B. Quinn JH et al. Mouth care guidance and support in cancer and palliative care. UK Oral Mucositis Cancer Gr. 2015;second edi(May):1-12.
3. Sroussi HY, Epstein JB, Bensadoun RJ, et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017. doi:10.1002/cam4.1221
4. Sonis ST, Elting LS, Keefe D, et al. Perspectives on Cancer Therapy-Induced Mucosal Injury: Pathogenesis, Measurement, Epidemiology, and Consequences for Patients. Cancer. 2004. doi:10.1002/cncr.20162
5. Silverman S. Diagnosis and management of oral mucositis. J Support Oncol. 2007.
6. Bensadoun RJ. Updated clinical practice guidelines for the prevention and treatment of mucositis. In: Proceedings of the 6th International Congress of the World Association of Laser Therapy, WALT 2006. ; 2006. doi:10.1002/cncr.22484
7. Epstein JB, Thariat J, Bensadoun RJ, et al. Oral complications of cancer and cancer therapy: From cancer treatment to survivorship. CA Cancer J Clin. 2012. doi:10.3322/caac.21157
8. Gautam AP, Fernandes DJ, Vidyasagar MS, Maiya AG, Nigudgi S. Effect of low-level laser therapy on patient reported measures of oral mucositis and quality of life in head and neck cancer patients receiving chemoradiotherapy – A randomized controlled trial. Support Care Cancer. 2013. doi:10.1007/s00520-012-1684-4
<< Back to Contents Menu
EDITOR’S PAGE | ADVISORY BOARD | NEWS | PRODUCTS | COVER FEATURE | CLINICAL | PROFILE | EXHIBITIONS & CONFERENCES | PRODUCT TIPS | DENTAL BUSINESS
9. Duncan GG, Epstein JB, Tu D, et al. Quality of life, mucositis, and xerostomia from radiotherapy for head and neck cancers: A report from the NCIC CTG HN2 randomized trial of an antimicrobial lozenge to prevent mucositis. Head Neck. 2005. doi:10.1002/hed.20162
10. Shankar A, Roy S, Bhandari M, et al. Current trends in management of oral mucositis in cancer treatment. Asian Pacific J Cancer Prev. 2017. doi:10.22034/APJCP.2017.18.8.2019
11. Hong CHL, Gueiros LA, Fulton JS, et al. Systematic review of basic oral care for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. July 2019. doi:10.1007/s00520-019-04848-4
12. Bezinelli LM, Eduardo FP, Neves VD, et al. Quality of life related to oral mucositis of patients undergoing haematopoietic stem cell transplantation and receiving specialised oral care with low-level laser therapy: a prospective observational study. Eur J Cancer Care (Engl). 2016;25(4). doi:10.1111/ecc.12344
13. Lalla R V., Bowen J, Barasch A, et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 2014;120(10):1453-1461. doi:10.1002/cncr.28592
14. Elting LS, Cooksley CD, Chambers MS, Garden AS. Risk, Outcomes, and Costs of Radiation-Induced Oral Mucositis Among Patients With Head-and-Neck Malignancies. Int J Radiat Oncol Biol Phys. 2007. doi:10.1016/j.ijrobp.2007.01.053
15. Sasportas LS, Hosford DN, Sodini MA, et al. Cost-effectiveness landscape analysis of treatments addressing xerostomia in patients receiving head and neck radiation therapy. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(1):e37-e51. doi:10.1016/j.oooo.2013.02.017
16. Dirix P, Nuyts S, Van Den Bogaert W. Radiation-induced xerostomia in patients with head and neck cancer: A literature review. Cancer. 2006;107(11):2525-2534. doi:10.1002/cncr.22302
17. Mester A, Mester A. The History of Photobiomodulation: Endre Mester (1903-1984). Photomed Laser Surg. 2017. doi:10.1089/pho.2017.4332
18. Anders JJ, Arany PR, Baxter GD, Lanzafame RJ. Light-emitting diode therapy and low-level light therapy are photobiomodulation therapy. Photobiomodulation, Photomedicine, Laser Surg. 2019;37(2):63-65. doi:10.1089/photob.2018.4600
19. Bensadoun RJ, Franquin JC, Ciais G, et al. Low-energy He/Ne laser in the prevention of radiation-induced mucositis: A multicenter phase III randomized study in patients with head and neck cancer. Support Care Cancer. 1999. doi:10.1007/s005200050256
20. Low-level laser therapy for preventing or treating or oral mucositis caused by radiotherapy or chemotherapy. 2018:1-4. http://nice.org.uk/guidance/ipg615.
21. Al-Rudayni AHM, Gopinath D, Maharajan MK, Veettil SK, Menon RK. Efficacy of photobiomodulation in the treatment of cancer chemotherapy-induced oral mucositis: A meta-analysis with trial sequential analysis. Int J Environ Res Public Health. 2021;18(14). doi:10.3390/ijerph18147418
22. Bjordal JM, Bensadoun RJ, Tunèr J, Frigo L, Gjerde K, Lopes-Martins RA. A systematic review with meta-analysis of the effect of low-level laser therapy (LLLT) in cancer therapy-induced oral mucositis. Support Care Cancer. 2011;19(8):1069-1077. doi:10.1007/s00520-011-1202-0
23. de Lima VHS, de Oliveira-Neto OB, da Hora Sales PH, da Silva Torres T, de Lima FJC. Effectiveness of low-level laser therapy for oral mucositis prevention in patients undergoing chemoradiotherapy for the treatment of head and neck cancer: A systematic review and meta-analysis. Oral Oncol. 2020;102. doi:10.1016/j.oraloncology.2019.104524
24. He M, Zhang B, Shen N, Wu N, Sun J. A systematic review and meta-analysis of the effect of low-level laser therapy (LLLT) on chemotherapy-induced oral mucositis in pediatric and young patients. Eur J Pediatr. 2018. doi:10.1007/s00431-017-3043-4
25. Mazhari F, Shirazi AS, Shabzendehdar M. Management of oral mucositis in pediatric patients receiving cancer therapy: A systematic review and meta-analysis. Pediatr Blood Cancer. 2019;66(3). doi:10.1002/pbc.27403
26. Marín-Conde F, Castellanos-Cosano L, Pachón-Ibañez J, Serrera-Figallo MA, Gutiérrez-Pérez JL, Torres-Lagares D. Photobiomodulation with low-level laser therapy reduces oral mucositis caused by head and neck radio-chemotherapy: prospective randomized controlled trial. Int J Oral Maxillofac Surg. 2019;48(7):917-923. doi:10.1016/j.ijom.2018.12.006
27. Zadik Y, Arany PR, Fregnani ER, et al. Systematic review of photobiomodulation for the management of oral mucositis in cancer patients and clinical practice guidelines. Support Care Cancer. July 2019. doi:10.1007/s00520-019-04890-2
28. Robijns J, Nair RG, Lodewijckx J, et al. Photobiomodulation therapy in management of cancer therapy-induced side effects: WALT position paper 2022. Front Oncol. 2022;12(August). doi:10.3389/fonc.2022.927685
29. Elad S, Arany P, Bensadoun RJ, Epstein JB, Barasch A, Raber-Durlacher J. Photobiomodulation therapy in the management of oral mucositis: search for the optimal clinical treatment parameters. Support Care Cancer. 2018. doi:10.1007/s00520-018-4262-6
30. da Silva BM, Prosdócimo ML, Gasparini LR, da Silva BM, de Araujo MR, Amenábar JM. Most used photobiomodulation dosimetry parameters to treat oral mucositis after preconditioning for hematopoietic stem cell transplantation: systematic review and meta-analysis. Support Care Cancer. 2022;30(5):3721-3732. doi:10.1007/s00520-022-06817-w
The information and viewpoints presented in the above news piece or article do not necessarily reflect the official stance or policy of Dental Resource Asia or the DRA Journal. While we strive to ensure the accuracy of our content, Dental Resource Asia (DRA) or DRA Journal cannot guarantee the constant correctness, comprehensiveness, or timeliness of all the information contained within this website or journal.
Please be aware that all product details, product specifications, and data on this website or journal may be modified without prior notice in order to enhance reliability, functionality, design, or for other reasons.
The content contributed by our bloggers or authors represents their personal opinions and is not intended to defame or discredit any religion, ethnic group, club, organisation, company, individual, or any entity or individual.